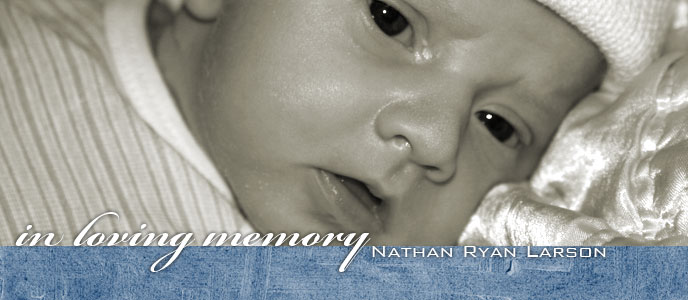
On Sunday, March 30th, 2008, our dear son Nathan Ryan Larson went home to our Lord in heaven. His twenty five days here with us were precious beyond words. Many of our friends and family followed Nate's story as he battled for his life. Much of his journey was depicted in 25 days of email updates, photos and video.
Nate's journey was an extraordinary one. We invite you to honor his short life with us, by reading through his journey in a thread of email updates, in photos and in video.
We deeply appreciate the outpouring of love and support from our family and friends, and invite you to leave your thoughts and prayers by commenting below.
In loving memory of Nate,
Erik, Trisha, Shayna, Noah, Kyla, and Kaylee Larson
To leave us your comments, thoughts and prayers, click on the link "COMMENTS" below. Please remember to include your name.
Nate's Journey in Photos
Just above the small thumb images of Nathan, you'll see the word "Notes." Roll your mouse pointer over that for a description of each photo.
Nate's Journey in Email
Nate's journey was journaled in a sequence of email updates, going all the way back to August of 2007. We invite you to download the PDF below and read through his story, or just scroll down.
Download a PDF of Nate's email here.
August 8, 2007
I wanted to let you all know that we will be adding a 7th family member. Baby #5 is due the end of March!
(Anticipated) FAQ'S - Frequently asked questions
Are you crazy?
Yes, absolutely, without a doubt.
What were you thinking?
Actually, we've been thinking about this for almost 3 years. After I had the twins I completely expected to have that "done" feeling, but I didn't. Driving home from the hospital, Erik commented that we still had 2 seats in the Suburban and we both just felt like someone was missing. We decided to wait 3 years and then make a final decision. I spent much of that time praying that this desire would go away. 5 kids is a crazy thought! But it never did. I just always felt like this was some sort of calling from God and that I would forever regret the decision if we closed the door. So, in June we decided to open the door and let God decide on what family he wanted us to have. We DEFINITELY weren't trying but now we weren't preventing. With all of our other kids, it took a long time and a lot of effort for us to get pregnant. So, we were SHOCKED to discover that we were pregnant 1 month later. We really feel that this was God's plan for us.
Are you sure that there's only 1?
Yes, we had an ultrasound and there is only 1 heartbeat (thank goodness)!
Are you freaking out?
Yes, a little bit. It's 5 kids! But when we told Shayna she started crying and said that God answered her prayer because she had been praying for a baby. That helps ease the shock a little.
Will you ever leave the house again?
I have to. I have 4 kids in school, soccer, gymnastics, Girl Scouts etc. Hopefully this kid will be easy going because it's going to be carted around a lot.
Do you have the "DONE" feeling yet?
Yes, absolutely. The minute the pee stick was positive!
Hope you're all having a great Summer and I hope to see you soon!
Love, Trisha (your crazy friend with 5 kids)
(Anticipated) FAQ'S - Frequently asked questions
Are you crazy?
Yes, absolutely, without a doubt.
What were you thinking?
Actually, we've been thinking about this for almost 3 years. After I had the twins I completely expected to have that "done" feeling, but I didn't. Driving home from the hospital, Erik commented that we still had 2 seats in the Suburban and we both just felt like someone was missing. We decided to wait 3 years and then make a final decision. I spent much of that time praying that this desire would go away. 5 kids is a crazy thought! But it never did. I just always felt like this was some sort of calling from God and that I would forever regret the decision if we closed the door. So, in June we decided to open the door and let God decide on what family he wanted us to have. We DEFINITELY weren't trying but now we weren't preventing. With all of our other kids, it took a long time and a lot of effort for us to get pregnant. So, we were SHOCKED to discover that we were pregnant 1 month later. We really feel that this was God's plan for us.
Are you sure that there's only 1?
Yes, we had an ultrasound and there is only 1 heartbeat (thank goodness)!
Are you freaking out?
Yes, a little bit. It's 5 kids! But when we told Shayna she started crying and said that God answered her prayer because she had been praying for a baby. That helps ease the shock a little.
Will you ever leave the house again?
I have to. I have 4 kids in school, soccer, gymnastics, Girl Scouts etc. Hopefully this kid will be easy going because it's going to be carted around a lot.
Do you have the "DONE" feeling yet?
Yes, absolutely. The minute the pee stick was positive!
Hope you're all having a great Summer and I hope to see you soon!
Love, Trisha (your crazy friend with 5 kids)
November 1, 2007
Family/Friends:
I know that email is not the most personal way to deliver this request, but it's difficult to talk about it--as you can imagine, and I wanted to get as many people praying ASAP.
Trisha and I just returned from the perinatologist for an ultrasound on the yet to be named Larson. She discovered a major heart defect which, if correctable, will require surgery after birth. There is a problem with the ventricles--there's only one instead of 2. Initial diagnosis is "Tetralogy of Fallot." We don't know much more than that, and we are lining up appointments with specialists to get a more definitive diagnosis/prognosis. Trisha will likely get an amniocentesis on Monday to check for genetic problems (this would mean a false negative from the blood work already done).
Please pray for a miracle healing. Pray that whatever the official diagnosis is, that it's correctable. Pray for our family--Shayna & Noah especially as they are old enough to know something is wrong. Also Trisha & me as we cope with this.
Also, feel free to forward this to others who you think would be willing to pray.
Thank you so much!
Erik
I know that email is not the most personal way to deliver this request, but it's difficult to talk about it--as you can imagine, and I wanted to get as many people praying ASAP.
Trisha and I just returned from the perinatologist for an ultrasound on the yet to be named Larson. She discovered a major heart defect which, if correctable, will require surgery after birth. There is a problem with the ventricles--there's only one instead of 2. Initial diagnosis is "Tetralogy of Fallot." We don't know much more than that, and we are lining up appointments with specialists to get a more definitive diagnosis/prognosis. Trisha will likely get an amniocentesis on Monday to check for genetic problems (this would mean a false negative from the blood work already done).
Please pray for a miracle healing. Pray that whatever the official diagnosis is, that it's correctable. Pray for our family--Shayna & Noah especially as they are old enough to know something is wrong. Also Trisha & me as we cope with this.
Also, feel free to forward this to others who you think would be willing to pray.
Thank you so much!
Erik
November 7, 2007
Family & friends:
Trisha and I want to thank you for your prayers and unbelievable support. This has been the hardest week of our life. Since we learned the newest Larson has a heart defect, we have been back to the doctor twice; once to the perinatologist for the amniocentesis, and once to the Cardiologist at CHOC for ultrasound. The amniocentesis result will confirm whether or not a genetic defect is present (1st trimester blood test was negative). Results are due next week. The cardiologist provided us with a diagnosis of "Tetrology of Fallot Pulmonary Atresia Ventricular Septal Defect." In english, the pulminary arteries are not visable on ultrasound (could be there--just too small to see now), the vessel from the right ventrical to the pulmonary artery is not there, and there is a defect in the septum which separates the right ventrical from the left. This is not a rock solid diagnosis, because the anatomy of the heart is so tiny right now. We are going back in early January for another ultrasound & hope to get a more definitive diagnosis. We were told that the most accurate diagnosis will come once the baby is delivered.
We are expected to have an otherwise normal pregnancy (closely monitored by perinatologist), and a normal delivery (c-section not required). We will likely deliver @ St. Joseph/CHOC in Orange sometime in March. The baby is expected to go directly to NICU for final diagnosis with possible heart surgery the first week. The baby is then expected to spend 2-4 weeks in the NICU before returning home. Repair for this condition will require multiple surgeries. The next surgery will likely be within the first year--probably 6-8 months. Travel to Stanford to a surgeon who specializes in this condition is expected. Along with several other anatomy elements to be repaired, this condition requires a "conduit," which is a tube with a valve in it. It will have to be replaced to keep up with the size of the heart. It will also have to be maintained if/when it calcifies. As for survival odds--we don't know yet. That depends almost entirely on the anatomy of the heart which cannot be seen as well in utero. The pending genetic test outcome will also drive the survival odds. This all sounds really negative, but there is hope! Our cardiologist says patients can lead a normal life after this type of repair. Also, the article below indicates, "In patients with operable pulmonary arteries, survival rates with satisfactory quality of life now reach 90%." The doctor at Stanford has had experience doing surgery where the pulmonary arteries are diminutive.
Please continue to pray for the baby, and for our family. Please pray for God to give us wisdom to make the right choices for doctors/hospitals.
With Love,
Erik & Trisha
Trisha and I want to thank you for your prayers and unbelievable support. This has been the hardest week of our life. Since we learned the newest Larson has a heart defect, we have been back to the doctor twice; once to the perinatologist for the amniocentesis, and once to the Cardiologist at CHOC for ultrasound. The amniocentesis result will confirm whether or not a genetic defect is present (1st trimester blood test was negative). Results are due next week. The cardiologist provided us with a diagnosis of "Tetrology of Fallot Pulmonary Atresia Ventricular Septal Defect." In english, the pulminary arteries are not visable on ultrasound (could be there--just too small to see now), the vessel from the right ventrical to the pulmonary artery is not there, and there is a defect in the septum which separates the right ventrical from the left. This is not a rock solid diagnosis, because the anatomy of the heart is so tiny right now. We are going back in early January for another ultrasound & hope to get a more definitive diagnosis. We were told that the most accurate diagnosis will come once the baby is delivered.
We are expected to have an otherwise normal pregnancy (closely monitored by perinatologist), and a normal delivery (c-section not required). We will likely deliver @ St. Joseph/CHOC in Orange sometime in March. The baby is expected to go directly to NICU for final diagnosis with possible heart surgery the first week. The baby is then expected to spend 2-4 weeks in the NICU before returning home. Repair for this condition will require multiple surgeries. The next surgery will likely be within the first year--probably 6-8 months. Travel to Stanford to a surgeon who specializes in this condition is expected. Along with several other anatomy elements to be repaired, this condition requires a "conduit," which is a tube with a valve in it. It will have to be replaced to keep up with the size of the heart. It will also have to be maintained if/when it calcifies. As for survival odds--we don't know yet. That depends almost entirely on the anatomy of the heart which cannot be seen as well in utero. The pending genetic test outcome will also drive the survival odds. This all sounds really negative, but there is hope! Our cardiologist says patients can lead a normal life after this type of repair. Also, the article below indicates, "In patients with operable pulmonary arteries, survival rates with satisfactory quality of life now reach 90%." The doctor at Stanford has had experience doing surgery where the pulmonary arteries are diminutive.
Please continue to pray for the baby, and for our family. Please pray for God to give us wisdom to make the right choices for doctors/hospitals.
With Love,
Erik & Trisha
November 27, 2007
Family & friends:
We wanted to keep you in the loop as developments happen. We got some good news yesterday on the genetic testing. The final test results came back normal. This is good news because genetic problems drive down the survival rates. No new news on the heart defect. We expect to have more information following the next series of scans to be done in early January.
Thank you all again for your support. Please continue to pray.
With Love, Erik & Trisha
We wanted to keep you in the loop as developments happen. We got some good news yesterday on the genetic testing. The final test results came back normal. This is good news because genetic problems drive down the survival rates. No new news on the heart defect. We expect to have more information following the next series of scans to be done in early January.
Thank you all again for your support. Please continue to pray.
With Love, Erik & Trisha
January 9, 2008
Dear Family and Friends,
We were waiting to send out another update until we had finalized some decisions and had more to report. It has since become obvious to us that we need support and prayer in making these decisions -- they are not coming easy to us. Since our last update, we've consulted with the surgeon at Stanford, had another set of electrocardiograms with the CHOC cardiologist and had multiple visits with our Perinatologist.
*Dr. Hanley (Stanford Cardiothoracic Surgeon)-* In mid Dec. we had a phone consultation with Dr. Hanley (a CD of our echo cardiogram and images were sent to him in Nov.). From our research and our Cardiologist's recommendations, Dr. Hanley appears to be the best surgeon for our particular heart defect. He has done over 400 similar surgeries (of significantly varying degrees) in the last 15 years and currently has a 90+% survival rate. He confirmed the diagnosis made by our Cardiologist (Tetrology of Fallot w/ Pulmonary Atresia) and said that based on the images, he did not feel that our baby had a pulmonary artery as well (something our Cardioligist suspected). This will not be confirmed until the baby is delivered. Once the baby is born, it will undergo a Cardiac Catheterization procedure in the first couple days of life. This involves putting the baby under anesthesia and inserting a material into the blood and running a catheter into the heart so that blood vessels can be identified accurately. If there is blood flow through the pulmonary artery (provides blood from the heart to the lungs) , surgery will need to be done within the first week to keep that vessel open (it naturally closes after birth). This surgeon believes in repairing the artery and the entire heart defect at the same time. Other surgeons believe that it's best to insert a shunt (a plastic part that keeps the artery open for blood flow) during the first week and then do another surgery several months later to repair the other defects. Dr. Hanley believes that there is a 10-15% chance that our baby will need surgery the first week. He believes that it is likely that our baby has collateral arteries (small arteries that the baby developed to compensate for the missing pulmonary artery). In this situation, he would stabilize the baby and send it home until the baby is 3-4 months old when the repair surgery would be optimal. Of course, if our Cardiologist determines that the baby is in distress, surgery could be done at any time during the first 4 months. Because of the collateral arteries, our repair surgery is extremely complicated. The surgeon has to connect the small collateral arteries together to make 1 functional pulmonary artery and then connect that to the heart and each lung. Then place a conduit between the Right Ventricle and this newly created vessel to the lungs, and patch the hole (VSD) between right and left ventricle. He classifies it as a 9 or 10 in severity/complexity out of a possible 10. During our consultation he informed us that it would be best to deliver the baby at Stanford so that if surgery is needed the first week (10-15% chance), so we would not need to transport a fragile newborn which can be more dangerous than the actual surgery.
*2nd echo cardiogram with Cardiologist -* We met with our cardiologist at CHOC again last week. At this time she still does not see any evidence of a pulmonary artery. Rather, she sees 3 small collateral arteries that appear to connect from the heart to the lungs. There could be other collaterals as well that are smaller and not visible (the more collaterals there are, the more complicated the repair is). There is a remote chance that there could also still be a pulmonary artery, however there is no evidence of that at this time. She informed us that we could still deliver at CHOC since surgery the first week is unlikely but the surgeon at CHOC is not qualified to perform our repair surgery. She referred us to another surgeon at Children's Hospital LA for a consultation. We are meeting with him on Jan. 21st.
*Perinatologist *- All of our regular appointments show that the baby is doing well in the womb and is growing accordingly (finally some good news). As of today, the baby is estimating a weight of over 3 pounds and all other organs appear to be fine. We will start fetal monitoring twice a week at 32 weeks and continue weekly ultrasounds to monitor growth and development.
We are currently in our 30th week. We need to decide on a hospital/surgeon ASAP. After our consultation with Dr. Hanley we felt that it made sense to deliver the baby at Stanford. However, since then, we've vacillated.
*The pros we've identified are:
* Dr. Hanley is the most qualified surgeon for our condition and we want our baby to be in the very best hands. * Lucile Packard Children's Hospital (Stanford) is the #11 children's hospital in the country and specializes in dealing with heart defects.
* The cons we've identified are:
* They want Trisha up at Stanford between 36-37 weeks of pregnancy - much sooner than we expected. She would likely travel up there with the twins and her mom. Erik would stay home with Shayna and Noah for a week or two until the due date got closer. They would likely induce at 39 weeks.
* The Ronald McDonald house that we planned on staying at (only $10 per night) will only accommodate a family of 4 and availability is not guaranteed. This means that we would need to rent a hotel room for at least part of our stay.
* We only have 1 family car and would need to rent a minivan for 3-4 weeks for Stanford.
* Based on the last echo cardiogram, surgery is not likely the first week so we would deliver the baby and return for surgery at a later date. We could deliver at CHOC or Children's Hospital LA which would be a lot less complicated logistically.
We've already switched to a PPO which is quite expensive but will allow us the freedom of choosing our doctors and hospitals. So the decision is truly ours. We don't want any of our decisions to be made from a financial standpoint. We would spend any amount of money necessary to save our baby's life. That being said, we don't want to use our resources unnecessarily. So, we would really appreciate it if anyone has connections that can help us out with our travel expenses should we decide to deliver at Stanford. If you know anyone at the following companies, please let us know:
/Airlines -/ Southwest and American have the most availability with flights from Orange County to San Jose. Erik will likely fly back and forth 1 or 2 times with Shayna and Noah to help keep their lives normal with school/sports. Since we aren't certain of any dates, we can't purchase tickets ahead of time at lower rates.
/Car Rental -/ we will likely need to rent a minivan for 3-4 weeks and would appreciate a reduced rate.
/Hotels -/ We would need to stay in a hotel for 3-4 weeks up at Stanford for delivery and again for the surgery likely this Summer.
*Decisions, Decisions... *
Our choices seem to be
1. Deliver at CHOC, and run the risk of immediate surgery being required (less than 15%)--which means transport to Stanford in an airborne NICU. If there is no need for immediate surgery--we go home and travel to Stanford sometime in the first 3-4 months for surgery. 2. Deliver at CHLA, and run the risk of immediate surgery being required--maybe by the CHLA surgeon--maybe transport to Stanford--depending on what he has to say when we meet with him on the 21st of this month.
3. Deliver at LPCH, and incur the logistic challenge--this seems to be the best scenario for the baby if surgery is required right away.
Sorry for the long/detailed email. We wanted to share our experiences so that you can pray with knowledge. Please pray for direction as there are so many options and unknowns. And please continue to pray for our baby. We have a very long and difficult road ahead of us.
With love,
Erik & Trisha
We were waiting to send out another update until we had finalized some decisions and had more to report. It has since become obvious to us that we need support and prayer in making these decisions -- they are not coming easy to us. Since our last update, we've consulted with the surgeon at Stanford, had another set of electrocardiograms with the CHOC cardiologist and had multiple visits with our Perinatologist.
*Dr. Hanley (Stanford Cardiothoracic Surgeon)-* In mid Dec. we had a phone consultation with Dr. Hanley (a CD of our echo cardiogram and images were sent to him in Nov.). From our research and our Cardiologist's recommendations, Dr. Hanley appears to be the best surgeon for our particular heart defect. He has done over 400 similar surgeries (of significantly varying degrees) in the last 15 years and currently has a 90+% survival rate. He confirmed the diagnosis made by our Cardiologist (Tetrology of Fallot w/ Pulmonary Atresia) and said that based on the images, he did not feel that our baby had a pulmonary artery as well (something our Cardioligist suspected). This will not be confirmed until the baby is delivered. Once the baby is born, it will undergo a Cardiac Catheterization procedure in the first couple days of life. This involves putting the baby under anesthesia and inserting a material into the blood and running a catheter into the heart so that blood vessels can be identified accurately. If there is blood flow through the pulmonary artery (provides blood from the heart to the lungs) , surgery will need to be done within the first week to keep that vessel open (it naturally closes after birth). This surgeon believes in repairing the artery and the entire heart defect at the same time. Other surgeons believe that it's best to insert a shunt (a plastic part that keeps the artery open for blood flow) during the first week and then do another surgery several months later to repair the other defects. Dr. Hanley believes that there is a 10-15% chance that our baby will need surgery the first week. He believes that it is likely that our baby has collateral arteries (small arteries that the baby developed to compensate for the missing pulmonary artery). In this situation, he would stabilize the baby and send it home until the baby is 3-4 months old when the repair surgery would be optimal. Of course, if our Cardiologist determines that the baby is in distress, surgery could be done at any time during the first 4 months. Because of the collateral arteries, our repair surgery is extremely complicated. The surgeon has to connect the small collateral arteries together to make 1 functional pulmonary artery and then connect that to the heart and each lung. Then place a conduit between the Right Ventricle and this newly created vessel to the lungs, and patch the hole (VSD) between right and left ventricle. He classifies it as a 9 or 10 in severity/complexity out of a possible 10. During our consultation he informed us that it would be best to deliver the baby at Stanford so that if surgery is needed the first week (10-15% chance), so we would not need to transport a fragile newborn which can be more dangerous than the actual surgery.
*2nd echo cardiogram with Cardiologist -* We met with our cardiologist at CHOC again last week. At this time she still does not see any evidence of a pulmonary artery. Rather, she sees 3 small collateral arteries that appear to connect from the heart to the lungs. There could be other collaterals as well that are smaller and not visible (the more collaterals there are, the more complicated the repair is). There is a remote chance that there could also still be a pulmonary artery, however there is no evidence of that at this time. She informed us that we could still deliver at CHOC since surgery the first week is unlikely but the surgeon at CHOC is not qualified to perform our repair surgery. She referred us to another surgeon at Children's Hospital LA for a consultation. We are meeting with him on Jan. 21st.
*Perinatologist *- All of our regular appointments show that the baby is doing well in the womb and is growing accordingly (finally some good news). As of today, the baby is estimating a weight of over 3 pounds and all other organs appear to be fine. We will start fetal monitoring twice a week at 32 weeks and continue weekly ultrasounds to monitor growth and development.
We are currently in our 30th week. We need to decide on a hospital/surgeon ASAP. After our consultation with Dr. Hanley we felt that it made sense to deliver the baby at Stanford. However, since then, we've vacillated.
*The pros we've identified are:
* Dr. Hanley is the most qualified surgeon for our condition and we want our baby to be in the very best hands. * Lucile Packard Children's Hospital (Stanford) is the #11 children's hospital in the country and specializes in dealing with heart defects.
* The cons we've identified are:
* They want Trisha up at Stanford between 36-37 weeks of pregnancy - much sooner than we expected. She would likely travel up there with the twins and her mom. Erik would stay home with Shayna and Noah for a week or two until the due date got closer. They would likely induce at 39 weeks.
* The Ronald McDonald house that we planned on staying at (only $10 per night) will only accommodate a family of 4 and availability is not guaranteed. This means that we would need to rent a hotel room for at least part of our stay.
* We only have 1 family car and would need to rent a minivan for 3-4 weeks for Stanford.
* Based on the last echo cardiogram, surgery is not likely the first week so we would deliver the baby and return for surgery at a later date. We could deliver at CHOC or Children's Hospital LA which would be a lot less complicated logistically.
We've already switched to a PPO which is quite expensive but will allow us the freedom of choosing our doctors and hospitals. So the decision is truly ours. We don't want any of our decisions to be made from a financial standpoint. We would spend any amount of money necessary to save our baby's life. That being said, we don't want to use our resources unnecessarily. So, we would really appreciate it if anyone has connections that can help us out with our travel expenses should we decide to deliver at Stanford. If you know anyone at the following companies, please let us know:
/Airlines -/ Southwest and American have the most availability with flights from Orange County to San Jose. Erik will likely fly back and forth 1 or 2 times with Shayna and Noah to help keep their lives normal with school/sports. Since we aren't certain of any dates, we can't purchase tickets ahead of time at lower rates.
/Car Rental -/ we will likely need to rent a minivan for 3-4 weeks and would appreciate a reduced rate.
/Hotels -/ We would need to stay in a hotel for 3-4 weeks up at Stanford for delivery and again for the surgery likely this Summer.
*Decisions, Decisions... *
Our choices seem to be
1. Deliver at CHOC, and run the risk of immediate surgery being required (less than 15%)--which means transport to Stanford in an airborne NICU. If there is no need for immediate surgery--we go home and travel to Stanford sometime in the first 3-4 months for surgery. 2. Deliver at CHLA, and run the risk of immediate surgery being required--maybe by the CHLA surgeon--maybe transport to Stanford--depending on what he has to say when we meet with him on the 21st of this month.
3. Deliver at LPCH, and incur the logistic challenge--this seems to be the best scenario for the baby if surgery is required right away.
Sorry for the long/detailed email. We wanted to share our experiences so that you can pray with knowledge. Please pray for direction as there are so many options and unknowns. And please continue to pray for our baby. We have a very long and difficult road ahead of us.
With love,
Erik & Trisha
February 7, 2008
Dear Friends & Family-
First of all, thanks all of you for your prayers and offers to help. We really appreciate you and are comforted by your outpouring of love.
After much prayer and consideration, we have decided to deliver the baby near Children's Hospital L.A.(CHLA). We'll give you more details on our rationale as well as what we expect to happen with the delivery. We are providing this information because many of you have asked about it. would like to know and it's difficult for us to talk about time and time again. However, we apologize to those that just want an update without all of the details.
More Details:
First of all, we have been told that there are six surgeons in the US who are able to perform our surgery. Arguably, the best two are on the West Coast and we have met with both of them. We met Dr. Starnes at CHLA two weeks ago and toured the hospital. Dr. Starnes is a world renowned surgeon and is extremely qualified. While he does numerous complicated heart surgeries every week, he has performed less than 100 of our particular condition (Dr. Hanley at Stanford has done about 400). Starnes also has a very different opinion on how to repair our defect. He believes in doing the surgery in 2-3 stages as opposed to Hanley who does the entire repair at once. He agreed with our other doctors/surgeons that surgery is not likely the first week because there is no evidence of a pulmonary artery (/even though we would likely need immediate surgery, it would be much less complicated and our odds would be better if there were a pulmonary artery/). Given all we have learned & considering the impact on our family, we've decided to deliver at near CHLA. If, by chance, we need surgery the first week, Starnes is an expert and can perform the surgery. In addition, CHLA has an excellent cardiac unit and we are very comfortable with the staff. We still plan on travel to Palo Alto for repair surgery at Stanford with Dr. Hanley at a later date.
We will be delivering the baby next door to CHLA at Hollywood Presbyterian Hospital. We are meeting with a team of specialists in a couple of weeks that will orchestrate delivery and transfer the baby across the parking lot to CHLA. As of now, the plan is to induce labor between March 3rd & 10th (@38 weeks). Once born, the neonatal team will take the baby to the NICU for a few hours until it is stable enough to be transferred next door. The baby will be put on special medication as a precaution that requires a ventilator, IV fluids (no food for several days), and hooked up to several other tubes/machines (we'll spare you some detail). Erik can/will be with the baby the entire time. As soon as possible, a transfer team will take the baby to CHLA where it will go directly to the Cardiac Intensive Care Unit (CICU). There, the cardiac specialists will evaluate the baby and address any initial concerns. Erik will remain with the baby and Trisha is allowed to join as soon as she is able. They plan on performing a Cardiac Catheritization under anesthesia probably day 3 or 4. It will take several hours and there is a risk because the baby is a newborn and is already sick. At that point, we will meet with the surgeon and know exactly what the diagnosis/prognosis is. We have been told that there are 3 likely scenarios:
1. WORST CASE - There is no pulmonary artery and the collaterals are
not sufficient enough to repair. This is our worst nightmare as
surgery would not be an option and no repair is available.
2. BEST CASE- There is a pulmonary artery and they need to put in a
shunt to keep it open (temporary repair surgery performed at
CHLA). We would schedule the full-repair surgery for 2-8 months
later at Stanford.
3. MOST LIKELY-There is no pulmonary artery but the collaterals are
sufficient to repair in 2-6 months. The baby would be allowed to
come home after it's stable. It may require a feeding tube as
many babies with this condition have to use all their energy to
keep the blood pumping through their body. They're simply too
tired to suck and swallow. Others do fine and are able to breastfeed.
We are not planning on allowing visitors at the hospital. We will update via email as the situation develops. Erik can check email from his phone if you would like to contact us but we will be focused on our family and may not be able to return calls/emails. We will be sleeping in the CICU but will have a room at the Ronald McDonald House next door to shower/change. The kids will be at our house with family and we will bring them up to the Ronald McDonald House every 2 or 3 days so we can take turns spending time with them. The twins have never been away from us so this will be hard for them.
*Prayer Requests*
1. Pray that Trisha does not go into labor early.
2. Pray that the delivery goes smoothly.
3. Pray for the Cardiac Catheritization that requires anesthesia.
4. Pray that the baby has a pulmonary artery or substantial collateral arteries that are repairable.
5. Pray that we are able to bring the baby home in good condition with a good prognosis.
6. Pray for Shayna, Noah, Kyla & Kaylee. Their world is going to get ROCKED! Pray for comfort, understanding, and love during this difficult time.
7. Pray for Erik and Trisha--that we can hold it together with all of the chaos ensuing.
Thanks to all of you for your prayers and support. We appreciate that many of you want to help but there is simply nothing to do at this point except pray. We will update again once an induction date has been set and then from the hospital as the situation develops.
With love,
Erik & Trisha
First of all, thanks all of you for your prayers and offers to help. We really appreciate you and are comforted by your outpouring of love.
After much prayer and consideration, we have decided to deliver the baby near Children's Hospital L.A.(CHLA). We'll give you more details on our rationale as well as what we expect to happen with the delivery. We are providing this information because many of you have asked about it. would like to know and it's difficult for us to talk about time and time again. However, we apologize to those that just want an update without all of the details.
More Details:
First of all, we have been told that there are six surgeons in the US who are able to perform our surgery. Arguably, the best two are on the West Coast and we have met with both of them. We met Dr. Starnes at CHLA two weeks ago and toured the hospital. Dr. Starnes is a world renowned surgeon and is extremely qualified. While he does numerous complicated heart surgeries every week, he has performed less than 100 of our particular condition (Dr. Hanley at Stanford has done about 400). Starnes also has a very different opinion on how to repair our defect. He believes in doing the surgery in 2-3 stages as opposed to Hanley who does the entire repair at once. He agreed with our other doctors/surgeons that surgery is not likely the first week because there is no evidence of a pulmonary artery (/even though we would likely need immediate surgery, it would be much less complicated and our odds would be better if there were a pulmonary artery/). Given all we have learned & considering the impact on our family, we've decided to deliver at near CHLA. If, by chance, we need surgery the first week, Starnes is an expert and can perform the surgery. In addition, CHLA has an excellent cardiac unit and we are very comfortable with the staff. We still plan on travel to Palo Alto for repair surgery at Stanford with Dr. Hanley at a later date.
We will be delivering the baby next door to CHLA at Hollywood Presbyterian Hospital. We are meeting with a team of specialists in a couple of weeks that will orchestrate delivery and transfer the baby across the parking lot to CHLA. As of now, the plan is to induce labor between March 3rd & 10th (@38 weeks). Once born, the neonatal team will take the baby to the NICU for a few hours until it is stable enough to be transferred next door. The baby will be put on special medication as a precaution that requires a ventilator, IV fluids (no food for several days), and hooked up to several other tubes/machines (we'll spare you some detail). Erik can/will be with the baby the entire time. As soon as possible, a transfer team will take the baby to CHLA where it will go directly to the Cardiac Intensive Care Unit (CICU). There, the cardiac specialists will evaluate the baby and address any initial concerns. Erik will remain with the baby and Trisha is allowed to join as soon as she is able. They plan on performing a Cardiac Catheritization under anesthesia probably day 3 or 4. It will take several hours and there is a risk because the baby is a newborn and is already sick. At that point, we will meet with the surgeon and know exactly what the diagnosis/prognosis is. We have been told that there are 3 likely scenarios:
1. WORST CASE - There is no pulmonary artery and the collaterals are
not sufficient enough to repair. This is our worst nightmare as
surgery would not be an option and no repair is available.
2. BEST CASE- There is a pulmonary artery and they need to put in a
shunt to keep it open (temporary repair surgery performed at
CHLA). We would schedule the full-repair surgery for 2-8 months
later at Stanford.
3. MOST LIKELY-There is no pulmonary artery but the collaterals are
sufficient to repair in 2-6 months. The baby would be allowed to
come home after it's stable. It may require a feeding tube as
many babies with this condition have to use all their energy to
keep the blood pumping through their body. They're simply too
tired to suck and swallow. Others do fine and are able to breastfeed.
We are not planning on allowing visitors at the hospital. We will update via email as the situation develops. Erik can check email from his phone if you would like to contact us but we will be focused on our family and may not be able to return calls/emails. We will be sleeping in the CICU but will have a room at the Ronald McDonald House next door to shower/change. The kids will be at our house with family and we will bring them up to the Ronald McDonald House every 2 or 3 days so we can take turns spending time with them. The twins have never been away from us so this will be hard for them.
*Prayer Requests*
1. Pray that Trisha does not go into labor early.
2. Pray that the delivery goes smoothly.
3. Pray for the Cardiac Catheritization that requires anesthesia.
4. Pray that the baby has a pulmonary artery or substantial collateral arteries that are repairable.
5. Pray that we are able to bring the baby home in good condition with a good prognosis.
6. Pray for Shayna, Noah, Kyla & Kaylee. Their world is going to get ROCKED! Pray for comfort, understanding, and love during this difficult time.
7. Pray for Erik and Trisha--that we can hold it together with all of the chaos ensuing.
Thanks to all of you for your prayers and support. We appreciate that many of you want to help but there is simply nothing to do at this point except pray. We will update again once an induction date has been set and then from the hospital as the situation develops.
With love,
Erik & Trisha
February 21, 2008
Dear Friends & Family:
We met with the team of specialists at Hollywood Presbyterian Hospital this week that will be delivering our baby. At that time, we actually received good news. During our echo cardiograham, they were able to identify a pulmonary artery on our baby. They won't know how functional it is until after the catheterization procedure (they also see collaterals which suggests that it's very small) but the fact that it's there improves our surgical survival odds and baby's future quality of life prognosis. Based on this finding, they have already scheduled surgery for our baby to insert a temporary shunt. If the cardiac catheterization does not show blood flow through that artery, or the presence of a ductus arteriosus (basically a connection that allows blood to flow from the heart to the lungs), they will cancel it and wait to surgically repair the heart once the baby is a little bigger. As of now, the following are the schedule of dates targeted:
*Tuesday, March 4th* - Check into Hollywood Presbyterian for induction late evening.
*Wednesday, March 5th* - Labor induction and delivery of baby in early morning hours (baby to be transferred next door to CHLA once stable as previously described in last email).
*Thursday, March 6th* - Cardiac Catheterization Procedure (a little earlier than we wanted but this is the date that works best with the hospital and Cardiologists).
*Monday, March 10th* - SURGERY - Open heart surgery performed by Dr. Starnes to insert a temporary shunt in the pulmonary artery to maintain blood flow until the baby is bigger and the heart defect can be repaired.
We will update again if any of these dates change. Otherwise, we will email from the hospital as the situation develops. Once again, thanks to all of you for your prayers and support.
With love,
Erik & Trisha
PRAYER REQUESTS_
Pray that Trisha does not go into labor early./
Pray that the delivery goes smoothly and a c-section is NOT needed./
Pray that the baby is in good condition upon delivery (there's a HUGE degree of variance possible)./
Pray that the Cardiac Catherterization procedure on March 6th is successful and that the pulmonary artery is viable./
Pray that the surgery on March 10th (if needed) is successful./
Pray for Shayna, Noah, Kyla and Kaylee during the next few weeks. Pray for comfort, love and understanding./
Pray for Erik & Trisha. This is the most difficult time of our life. Pray for strength and comfort./
We met with the team of specialists at Hollywood Presbyterian Hospital this week that will be delivering our baby. At that time, we actually received good news. During our echo cardiograham, they were able to identify a pulmonary artery on our baby. They won't know how functional it is until after the catheterization procedure (they also see collaterals which suggests that it's very small) but the fact that it's there improves our surgical survival odds and baby's future quality of life prognosis. Based on this finding, they have already scheduled surgery for our baby to insert a temporary shunt. If the cardiac catheterization does not show blood flow through that artery, or the presence of a ductus arteriosus (basically a connection that allows blood to flow from the heart to the lungs), they will cancel it and wait to surgically repair the heart once the baby is a little bigger. As of now, the following are the schedule of dates targeted:
*Tuesday, March 4th* - Check into Hollywood Presbyterian for induction late evening.
*Wednesday, March 5th* - Labor induction and delivery of baby in early morning hours (baby to be transferred next door to CHLA once stable as previously described in last email).
*Thursday, March 6th* - Cardiac Catheterization Procedure (a little earlier than we wanted but this is the date that works best with the hospital and Cardiologists).
*Monday, March 10th* - SURGERY - Open heart surgery performed by Dr. Starnes to insert a temporary shunt in the pulmonary artery to maintain blood flow until the baby is bigger and the heart defect can be repaired.
We will update again if any of these dates change. Otherwise, we will email from the hospital as the situation develops. Once again, thanks to all of you for your prayers and support.
With love,
Erik & Trisha
PRAYER REQUESTS_
Pray that Trisha does not go into labor early./
Pray that the delivery goes smoothly and a c-section is NOT needed./
Pray that the baby is in good condition upon delivery (there's a HUGE degree of variance possible)./
Pray that the Cardiac Catherterization procedure on March 6th is successful and that the pulmonary artery is viable./
Pray that the surgery on March 10th (if needed) is successful./
Pray for Shayna, Noah, Kyla and Kaylee during the next few weeks. Pray for comfort, love and understanding./
Pray for Erik & Trisha. This is the most difficult time of our life. Pray for strength and comfort./
March 5, 2008
Family/Friends -
Induction started 4am today... no significant progress yet. Should be
born
today. Will update later after baby is born--when I can.
Pray for a cooperative baby (no C-section).
Thanks to everyone!
Erik & Trisha
Induction started 4am today... no significant progress yet. Should be
born
today. Will update later after baby is born--when I can.
Pray for a cooperative baby (no C-section).
Thanks to everyone!
Erik & Trisha
March 6, 2008
Everyone-
After a long, frustrating, complicated 18 hours of labor, BB Larson was born at 10:29pm last night--barely avoiding a c-section.. Weighing at a whopping 7#9oz, the baby came out kicking, & screaming. We are waiting to announce the sex until after we tell the kids tomorrow--we want them to be the first to know.
Baby is in the cardiothoracic ICU at CHLA after being brought 80 yards by ambulance from Hollywood Presbytarian hospital. Trisha is feeling great. We're very busy with lots of tests today & will update tomorrow with some results. We should have a name picked by then. Thanks all!
Love, Erik & Trisha
After a long, frustrating, complicated 18 hours of labor, BB Larson was born at 10:29pm last night--barely avoiding a c-section.. Weighing at a whopping 7#9oz, the baby came out kicking, & screaming. We are waiting to announce the sex until after we tell the kids tomorrow--we want them to be the first to know.
Baby is in the cardiothoracic ICU at CHLA after being brought 80 yards by ambulance from Hollywood Presbytarian hospital. Trisha is feeling great. We're very busy with lots of tests today & will update tomorrow with some results. We should have a name picked by then. Thanks all!
Love, Erik & Trisha
March 7, 2008
Please join us in celebrating the arrival of Nathan Ryan Larson! Born 3/5/2008 at 10:29pm, weighing in at 7lbs 9oz & 21". He met his brother and sisters this morning.
Nathan is stable, and receiving excellent care in the CTICU at CHLA. He has more tests scheduled today which will determine what repairs need to be made. We'll send out another update once we know more.
Thanks for all your prayers and continued support!
Erik & Trisha
Nathan is stable, and receiving excellent care in the CTICU at CHLA. He has more tests scheduled today which will determine what repairs need to be made. We'll send out another update once we know more.
Thanks for all your prayers and continued support!
Erik & Trisha
March 9, 2008

Dear Family and Friends -
Above is a picture of Nathan. His name means gift from God.
They removed the ventilator on Saturday, revealing his cute little face. We were able to hold him for the first time! Trisha waited until she was in physical pain to give him up after three hours of holding him. He is a bit puffy from the fluids used to manage his blood pressure, but that will return to normal after his surgery.
Friday he underwent a cardiac catheterrization. This is a catheter placed inside the heart under x-ray to map all anatomy. Our prayers for a pulmonary artery were answered! The artery, though imperfect and small, looks to be viable, and feeds all 15 sections of the lungs. This news changed the earlier diagnosis--dropping pulmonary atresia. Additionally, the vessel/valve which connect the right ventricle to the pulmonary artery (which we were told didn't exist) was clearly visible. Repair/replacement of this section will be needed in a few months as it is malformed.
His surgery is scheduled for Monday morning at 7am to place a shunt between the aorta and pulmonary artery. This increases blood flow in the proper direction, and should result in growth of the pulmonary artery. They may also close off abnormal vessels (collaterals) which route blood in the wrong direction.
The surgery and the 48 hours following surgery are critical, so please continue your prayers.
We will try to update tomorrow sometime after surgery.
Erik & Trisha
March 10, 2008
Baby Nate is getting closed now. The surgeon didn't put a shunt in, but modified the vessel from the rt ventricle to the pulmonary artery. This is great news as it allow for more uniform and normal blood flow which means a better chance for quality healing. Also less damage to the pulmonary artery. Also, he may be able to avoid an artificial conduit which means no need to replace an outgrown valve in the future. Nate will need at least one more surgery to close the hole between the ventricles and complete the repair started today. The collaterals were left open for now. These can be closed in the cathetarization lab later.
Please keep praying as the days after surgery are VERY critical.
Thank you for your prayers, they are working!!
Love Erik and Trisha
Please keep praying as the days after surgery are VERY critical.
Thank you for your prayers, they are working!!
Love Erik and Trisha
March 11, 2008
Family/Friends -
Nate's 1st full day after surgery was tough. He is sedated, & still on a ventilator. His vitals are, for the most part, steadily improving. He had a brief setback after they pulled out his chest tube. Apparently it's very painful & this caused a spike in his pulse and blood pressure. The plan is to slowly get him off the ventilator--we hope by Thursday--then reduce/eliminate as many of the other medications as possible while keeping all his vitals in check.
Please keep praying for his recovery, and our sanity.
Erik & Trisha
Nate's 1st full day after surgery was tough. He is sedated, & still on a ventilator. His vitals are, for the most part, steadily improving. He had a brief setback after they pulled out his chest tube. Apparently it's very painful & this caused a spike in his pulse and blood pressure. The plan is to slowly get him off the ventilator--we hope by Thursday--then reduce/eliminate as many of the other medications as possible while keeping all his vitals in check.
Please keep praying for his recovery, and our sanity.
Erik & Trisha
March 13, 2008
Quick update - Nate is expected to come off the ventilator today. He had a good day yesterday & is making steady progress.
Erik & Trisha
Erik & Trisha
March 13, 2008
Family/Friends -
Today did not go as expected. We feel like we are on a roller coaster and it's very obvious that we are not in control. The doctor's were hopeful that Nate would be ready to breathe on his own but when they tested him, he wasn't able. So, he did not come off the ventilator. We were very disappointed. Mostly because we just want to hold him. He gets another shot tomorrow morning, so please pray that he rallies and is ready to take this critical step. Thank you so much for your support!
Erik & Trisha
Today did not go as expected. We feel like we are on a roller coaster and it's very obvious that we are not in control. The doctor's were hopeful that Nate would be ready to breathe on his own but when they tested him, he wasn't able. So, he did not come off the ventilator. We were very disappointed. Mostly because we just want to hold him. He gets another shot tomorrow morning, so please pray that he rallies and is ready to take this critical step. Thank you so much for your support!
Erik & Trisha
March 14, 2008
Family/Friends -
Nate did not manage to get off the ventilator again today. There are several factors contributing to this being difficult--mostly he needs extra fluids to bolster his blood pressure, but these fluids make it difficult to maintain the ability to breathe on his own.
He'll try again tomorrow, so please pray that he is ready soon--if not off by next week he may need more changes to his anatomy (surgery or surgical procedure) before he will be able to breathe off the ventilator.
Also, please pray for his kidney health. Minor by comparison to everything else, but potentially another procedure to endure.
Thanks for all your feedback and words of support--they've been helpful.
Erik & Trisha
Nate did not manage to get off the ventilator again today. There are several factors contributing to this being difficult--mostly he needs extra fluids to bolster his blood pressure, but these fluids make it difficult to maintain the ability to breathe on his own.
He'll try again tomorrow, so please pray that he is ready soon--if not off by next week he may need more changes to his anatomy (surgery or surgical procedure) before he will be able to breathe off the ventilator.
Also, please pray for his kidney health. Minor by comparison to everything else, but potentially another procedure to endure.
Thanks for all your feedback and words of support--they've been helpful.
Erik & Trisha
March 15, 2008
Friends/Family -
Nathan came very close to getting off the ventilator (extubated) today. He was taken down to minimal settings where he breathes on his own with the tube in, but after a time, his blood gases dropped too low to continue. He was a close call, and we are hopeful that tomorrow he will do better.
Please pray that Nate will be strong enough to take this step tomorrow so he can get on with the next steps toward going home. Also, please pray for us, and the kids, as this was day 11 and everyone is wearing thin.
Thanks for everything!
Nathan came very close to getting off the ventilator (extubated) today. He was taken down to minimal settings where he breathes on his own with the tube in, but after a time, his blood gases dropped too low to continue. He was a close call, and we are hopeful that tomorrow he will do better.
Please pray that Nate will be strong enough to take this step tomorrow so he can get on with the next steps toward going home. Also, please pray for us, and the kids, as this was day 11 and everyone is wearing thin.
Thanks for everything!
March 16, 2008
Family/Friends -
Not yet... seems to be the theme over the weekend. Nathan couldn't muster the right scores on his blood gas tests to get off the ventilator. He'll try again tomorrow--please pray that he gets past this critical step as soon as possible.
Thanks for your support!
Erik & Trisha
Not yet... seems to be the theme over the weekend. Nathan couldn't muster the right scores on his blood gas tests to get off the ventilator. He'll try again tomorrow--please pray that he gets past this critical step as soon as possible.
Thanks for your support!
Erik & Trisha
March 17, 2008
Finally,we have good news to report. They pulled Nate's breathing tube almost exactly at 2:30 today. The first hour was pretty stressful, but after that, he figured it out and did really well. We just left the hospital -- he has been sleeping for the last 5 hours. Please continue to pray for him as there is still the possibility that his body will get tired and he will not be able to breathe without the help of the ventilator.
Assuming that all goes well throughout the night, tomorrow they will try and get him to take the next step. They will begin to eliminate his IV heart medications (currently on 4) and attempt to teach him how to bottle feed. They tell us that teaching them to suck, swallow and breathe simultaneously can prove difficult. He's been sucking on a pacifier the last few hours which is a good sign so we're hopeful that he'll pick it up easily.
Please pray that he continues to progress so that we can get closer to coming home. We long for the day that we can all be together under one roof again.
Erik & Trisha
Assuming that all goes well throughout the night, tomorrow they will try and get him to take the next step. They will begin to eliminate his IV heart medications (currently on 4) and attempt to teach him how to bottle feed. They tell us that teaching them to suck, swallow and breathe simultaneously can prove difficult. He's been sucking on a pacifier the last few hours which is a good sign so we're hopeful that he'll pick it up easily.
Please pray that he continues to progress so that we can get closer to coming home. We long for the day that we can all be together under one roof again.
Erik & Trisha
March 17, 2008
Family/Friends -
Happy St. Patrick's Day--though it seems a bit like Groundhog Day as we seem to encounter the same circumstances every day for the past 6 days or so. Today was supposed to be Nate's due date & we're hoping that today will include the luck of the Irish (the real Irish--not those domers from Indiana).
The important part: At about 2:30pm (pacific), they are going to pull the breathing tube & give Nathan a chance to breathe on his own. The testing to determine if he is ready is borderline--but they are giving him a shot to see how he responds. Please pray for him to be strong, and do well off the ventilator (both immediately and for the longer term--the 1st 24 hours off the vent are critical). If his vitals are not right, they will have to intubate again & this will extend his stay here in the hospital. They tell us that this is a painful process & we are really hoping to avoid it.
Thanks for your support.
Erik & Trisha
Happy St. Patrick's Day--though it seems a bit like Groundhog Day as we seem to encounter the same circumstances every day for the past 6 days or so. Today was supposed to be Nate's due date & we're hoping that today will include the luck of the Irish (the real Irish--not those domers from Indiana).
The important part: At about 2:30pm (pacific), they are going to pull the breathing tube & give Nathan a chance to breathe on his own. The testing to determine if he is ready is borderline--but they are giving him a shot to see how he responds. Please pray for him to be strong, and do well off the ventilator (both immediately and for the longer term--the 1st 24 hours off the vent are critical). If his vitals are not right, they will have to intubate again & this will extend his stay here in the hospital. They tell us that this is a painful process & we are really hoping to avoid it.
Thanks for your support.
Erik & Trisha
March 18, 2008
Family/Friends -
Today Nate stayed off the ventilator, and spent most of the day getting used to breathing on his own. Go Nathan!
On the flip side, we learned that both his kidneys are allowing urine to flow back into them from the bladder which can cause bacterial infections which are not good for his heart. Prophylactic antibiotics will be used to prevent infection until either the condition reverses itself or surgery is done to correct the problem (in a few months).
Beginning tonight, the doctors will ween him off the drugs. He'll need to be off most drugs (all I.V. drugs) before being ready to come home. Pray for Nate to get off of the vaporized oxygen as well. Once off I.V. drugs and the vapor machine, the focus will turn to eating. This could take 1-3 weeks--all dependent on Nate & his progress--so please pray for him to quickly adapt.
Thanks to all for your continued support & encouraging emails! :-)
Erik & Trisha
Today Nate stayed off the ventilator, and spent most of the day getting used to breathing on his own. Go Nathan!
On the flip side, we learned that both his kidneys are allowing urine to flow back into them from the bladder which can cause bacterial infections which are not good for his heart. Prophylactic antibiotics will be used to prevent infection until either the condition reverses itself or surgery is done to correct the problem (in a few months).
Beginning tonight, the doctors will ween him off the drugs. He'll need to be off most drugs (all I.V. drugs) before being ready to come home. Pray for Nate to get off of the vaporized oxygen as well. Once off I.V. drugs and the vapor machine, the focus will turn to eating. This could take 1-3 weeks--all dependent on Nate & his progress--so please pray for him to quickly adapt.
Thanks to all for your continued support & encouraging emails! :-)
Erik & Trisha
March 19, 2008
Family/Friends -
Nate has developed an infection and needs prayer for healing. There will be more information to come, but in the meantime the family has asked for your prayers. Thank you!
Nate has developed an infection and needs prayer for healing. There will be more information to come, but in the meantime the family has asked for your prayers. Thank you!
March 19, 2008
All - Nate couldn't breathe well enough on his own with the fever so he is back on the ventilator. He is stable, and his fever finally broke. Hopefully the doctors can find the source of infection and get it treated appropriately so he can get back on the path toward hospital discharge. Please pray that he will soon be ready to get back off the ventilator. Thanks for your prayers! We'll update again when we know more.
Erik & Trisha
Erik & Trisha
March 19, 2008
All -
The latest isn't great news. The infection is a blood infection, which on its own, is very serious. Its source was most likely one of the many IV tubes. Worst case is that it has embedded in the heart itself which would mean 4-6 weeks of IV antibiotics. Best case is the currently flowing antibiotics will knock it down quickly. He is still struggling with fever--the primary stats are still looking good (Blood pressure, heart rate, oxygen saturation, etc).
Please pray that he respond well to his medications, that the infection gets killed off quickly, and that Nate gets back off the ventilator soon.
Thanks for your support! Please forgive our being non-responsive to your emails--they are all read & very much appreciated. :-)
Erik & Trisha
The latest isn't great news. The infection is a blood infection, which on its own, is very serious. Its source was most likely one of the many IV tubes. Worst case is that it has embedded in the heart itself which would mean 4-6 weeks of IV antibiotics. Best case is the currently flowing antibiotics will knock it down quickly. He is still struggling with fever--the primary stats are still looking good (Blood pressure, heart rate, oxygen saturation, etc).
Please pray that he respond well to his medications, that the infection gets killed off quickly, and that Nate gets back off the ventilator soon.
Thanks for your support! Please forgive our being non-responsive to your emails--they are all read & very much appreciated. :-)
Erik & Trisha
March 20, 2008
All -
Today was slow & steady progress. Doctors discovered the source of the infection was from the urine flowing back to the kidneys from the bladder (which then got into the blood stream). The anti biotic did its thing--his fever is down and the tests for the infection are now negative. :) Because of the infection, the urology team wants to surgically repair the kidney/bladder problem as soon as possible. This could easily cause another infection which is life threatening with his compromised immune system. However, he is too little right now. They hope to schedule surgery when he is about 2 months (1st week of May).
The plan for tomorrow is to put in a picline (long term central IV) so that they can take out his central line which is now 10 days old and a potential source of infection. If that goes well and the infection continues to be managed they will make an attempt to get off the ventilator again as early as tomorrow afternoon. Because of the blood infection, Nate will require 10 days of IV antibiotics. So, he will be in the hospital at least 8 more days!
Please pray that the infection continues to be controlled and that he is able to get off the ventilator soon. He is 15 days old and we've only held him 3 times. Hospital days will be a lot more tolerable if we are able to hold him.
Thanks to all for your support & prayers.
Erik & Trisha
Today was slow & steady progress. Doctors discovered the source of the infection was from the urine flowing back to the kidneys from the bladder (which then got into the blood stream). The anti biotic did its thing--his fever is down and the tests for the infection are now negative. :) Because of the infection, the urology team wants to surgically repair the kidney/bladder problem as soon as possible. This could easily cause another infection which is life threatening with his compromised immune system. However, he is too little right now. They hope to schedule surgery when he is about 2 months (1st week of May).
The plan for tomorrow is to put in a picline (long term central IV) so that they can take out his central line which is now 10 days old and a potential source of infection. If that goes well and the infection continues to be managed they will make an attempt to get off the ventilator again as early as tomorrow afternoon. Because of the blood infection, Nate will require 10 days of IV antibiotics. So, he will be in the hospital at least 8 more days!
Please pray that the infection continues to be controlled and that he is able to get off the ventilator soon. He is 15 days old and we've only held him 3 times. Hospital days will be a lot more tolerable if we are able to hold him.
Thanks to all for your support & prayers.
Erik & Trisha
March 21, 2008
All -
Not a whole heck of a lot to report for today. Nate is holding steady--no progress, no regress. His infection is still present, though knocked down substantially by antibiotics. They attempted to take him off the ventilator again today--but he wasn't ready yet. He'll try again tomorrow. He spent most of the day sleeping after getting a new central line (PIC line). Please pray for overcoming this infection and successful removal from the ventilator.
Thanks all!
Erik & Trisha
Not a whole heck of a lot to report for today. Nate is holding steady--no progress, no regress. His infection is still present, though knocked down substantially by antibiotics. They attempted to take him off the ventilator again today--but he wasn't ready yet. He'll try again tomorrow. He spent most of the day sleeping after getting a new central line (PIC line). Please pray for overcoming this infection and successful removal from the ventilator.
Thanks all!
Erik & Trisha
Sunday, March 23, 2008 - Easter
Happy Easter all!
Sorry we didn't update yesterday. The kids are here for the weekend and we had a late night at the hospital.
Yesterday turned out to be a very good day. Nate looked a lot better in the morning. His color was back and he was moving around a lot like a normal newborn would (something he hasn't done yet). All his blood tests for the infection were significantly improved. The lab identified the infection as being E. coli. The doctors told us that this type of infection will put even the healthiest adult in the hospital so it's amazing that little Nathan (with his compromised immune system) recovered so well. They will continue to manage the infection and will put him on low dose antibiotics after these are finished until he has his kidney surgery.
They weaned him off of the ventilator yesterday morning and he looked great so at 3:20pm, they extubated (took it out). He did really well this time. He's been breathing faster than they would like but everything else looks great.
Today, Nate is still off the ventilator, and breathing only with the help of a vapo therm device (heated, pressurized, oxygenated air flowing through a nose plug thingy). No major changes planned for today--the plan is still to ween off his IV meds (only 1 left). Then tomorrow, they will try and ween off of the vapo therm. Once he is off that, they will start trying to feed him.
Nate is now 18 days old and we were able to hold him for the 4th time (hopefully the 5th tonight). Shayna was also able to hold him for the 1st time. It's been a very different Easter for us this year but getting the chance to hold him today made everything ok. Please pray that he continues to progress and move forward. Pray that he is able to slow down his breathing and eliminate his dependency on the vapo therm.
Blessings to all!
Erik & Trisha



Sorry we didn't update yesterday. The kids are here for the weekend and we had a late night at the hospital.
Yesterday turned out to be a very good day. Nate looked a lot better in the morning. His color was back and he was moving around a lot like a normal newborn would (something he hasn't done yet). All his blood tests for the infection were significantly improved. The lab identified the infection as being E. coli. The doctors told us that this type of infection will put even the healthiest adult in the hospital so it's amazing that little Nathan (with his compromised immune system) recovered so well. They will continue to manage the infection and will put him on low dose antibiotics after these are finished until he has his kidney surgery.
They weaned him off of the ventilator yesterday morning and he looked great so at 3:20pm, they extubated (took it out). He did really well this time. He's been breathing faster than they would like but everything else looks great.
Today, Nate is still off the ventilator, and breathing only with the help of a vapo therm device (heated, pressurized, oxygenated air flowing through a nose plug thingy). No major changes planned for today--the plan is still to ween off his IV meds (only 1 left). Then tomorrow, they will try and ween off of the vapo therm. Once he is off that, they will start trying to feed him.
Nate is now 18 days old and we were able to hold him for the 4th time (hopefully the 5th tonight). Shayna was also able to hold him for the 1st time. It's been a very different Easter for us this year but getting the chance to hold him today made everything ok. Please pray that he continues to progress and move forward. Pray that he is able to slow down his breathing and eliminate his dependency on the vapo therm.
Blessings to all!
Erik & Trisha



March 24, 2008
All -
Today was another good day for Nathan. His breathing slowed significantly and all other vitals are excellent. The doctors would like his breathing to slow a bit more, and ween him off the vapo therm. Over the weekend, they removed 3 of 4 IV lines and he is no longer on IV heart medicine. He's looking and acting more "normal" every day. Tomorrow, if vapo therm is low enough, he can bottle feed by Wednesday. Please pray that he continues to move forward and executes the suck/swallow/breathe successfully. Also pray that the infection stays knocked down.
Thanks all!
Erik & Trisha
Today was another good day for Nathan. His breathing slowed significantly and all other vitals are excellent. The doctors would like his breathing to slow a bit more, and ween him off the vapo therm. Over the weekend, they removed 3 of 4 IV lines and he is no longer on IV heart medicine. He's looking and acting more "normal" every day. Tomorrow, if vapo therm is low enough, he can bottle feed by Wednesday. Please pray that he continues to move forward and executes the suck/swallow/breathe successfully. Also pray that the infection stays knocked down.
Thanks all!
Erik & Trisha
March 26, 2008
EmailsFriends and Family -
Nathan's had a couple of pretty good days. His vapo therm is at minimum & we hope to take him off it tomorrow. He also started bottle feeding (1 Tbsp) with no problem! He did it on his first try--yeah, Nate! Because of the severity of the E. coli infection, doctors want to keep him on IV antibiotics until next Friday, so we are looking into transferring him south to CHOC so he can be closer to home. There's also a possibility that we can do the antibiotics with a home nurse & pull him out of the hospital early. Please pray that we are able to transfer to CHOC for this weekend and get a home care nurse for next week.
Thanks to all for your support!
Erik & Trisha
Nathan's had a couple of pretty good days. His vapo therm is at minimum & we hope to take him off it tomorrow. He also started bottle feeding (1 Tbsp) with no problem! He did it on his first try--yeah, Nate! Because of the severity of the E. coli infection, doctors want to keep him on IV antibiotics until next Friday, so we are looking into transferring him south to CHOC so he can be closer to home. There's also a possibility that we can do the antibiotics with a home nurse & pull him out of the hospital early. Please pray that we are able to transfer to CHOC for this weekend and get a home care nurse for next week.
Thanks to all for your support!
Erik & Trisha
March 27, 2008
Family & Friends -
Today, Nate and I took a helicopter (that's "helodocter" if you ask Noah) transport from CHLA to CHOC. Now Nate is only 22 miles from home which means no more Ronald McDonald house, no more LA traffic, and more time at home for the family! This was also Nate's best day so far. His vitals are great, he is eating well (mom's milk via bottle), he is on room air (still flowing with a nasal cannula), is on IV antibiotics, and only two heart medicines (these are long term which he'll stay on)--he seems very content. :-)
For those who have expressed a desire to visit--he is still in the ICU, so we're not allowing visitors just yet. Please pray for him to get up to full meals tomorrow as planned & that he can make enough progress to come home next week with a home care nurse.
Thanks to all for your continued support!
Erik & Trisha





Today, Nate and I took a helicopter (that's "helodocter" if you ask Noah) transport from CHLA to CHOC. Now Nate is only 22 miles from home which means no more Ronald McDonald house, no more LA traffic, and more time at home for the family! This was also Nate's best day so far. His vitals are great, he is eating well (mom's milk via bottle), he is on room air (still flowing with a nasal cannula), is on IV antibiotics, and only two heart medicines (these are long term which he'll stay on)--he seems very content. :-)
For those who have expressed a desire to visit--he is still in the ICU, so we're not allowing visitors just yet. Please pray for him to get up to full meals tomorrow as planned & that he can make enough progress to come home next week with a home care nurse.
Thanks to all for your continued support!
Erik & Trisha





March 29, 2008
Friends & Family -
Nate has had two great days @ CHOC. His oxygen and feeding tubes are now out. He only has his IV now (which he'll go home with). Yesterday and today he has been taking full feeds (2oz). If he continues to do this, he may get home this week! We're doing an extra week of IV antibiotics in case as if he had spinal meningitis. This is because they didn't do a spinal tap to test when his infection was active, so they are treating him as if he tested positive.
Please pray that he continues to feed well and he is discharged soon. We reeeeeally want to go home. Thanks for everything!
Erik & Trisha
Nate has had two great days @ CHOC. His oxygen and feeding tubes are now out. He only has his IV now (which he'll go home with). Yesterday and today he has been taking full feeds (2oz). If he continues to do this, he may get home this week! We're doing an extra week of IV antibiotics in case as if he had spinal meningitis. This is because they didn't do a spinal tap to test when his infection was active, so they are treating him as if he tested positive.
Please pray that he continues to feed well and he is discharged soon. We reeeeeally want to go home. Thanks for everything!
Erik & Trisha
March 30, 2008
Friends & Family -
Our hearts are broken. After only 25 days, Nathan Ryan has gone home to heaven. He was doing so great, and supposed to come home tomorrow, but took a terrible turn late this morning. We don't know what to do now--it's so hard. Please pray for our family.
Erik
Our hearts are broken. After only 25 days, Nathan Ryan has gone home to heaven. He was doing so great, and supposed to come home tomorrow, but took a terrible turn late this morning. We don't know what to do now--it's so hard. Please pray for our family.
Erik
April 3, 2008 - Nathan's Memorial Service
Today we paid tribute to Nathan's life. Someone made an audio recording, which is posted here.
Click here to listen to the audio
Click here to listen to the audio
June 11, 2008
The last 3 months have been extremely difficult. Not only have we been attempting to deal with our own pain, but that of our kids, and managing friends/family at the same time. There are so many people that want to know the answers to why Nate died? and how are we doing? We thought that it would be easier to just put it in writing so that people would understand what we're going through. We realize that this is a lengthy read, but we're hoping that it will give you some insight into our lives at the moment.
While we were at CHLA, we tried to keep our email updates positive--but those 3 weeks were excruciating. After an 18 hour, 98% natural labor, Trisha ran a marathon trying to save Nathan's life. She spent 16-19 hours everyday sitting on an uncomfortable office chair next to Nathan, caressing his head (because he had tubes everywhere else) and telling him how much she loved him. Those hours were extremely stressful--starring at his monitors and as alarms went off throughout the day & night, and holding her breath as the doctors and nurses adjusted medications and machine settings to keep him alive. The staff worked around the clock caring for him. The (Cardio Thoracic Intensive Care Unit) CTICU was insane. There were critically ill babies all around recovering from open heart surgery. Alarms and bells went off around the clock--Nathan was extremely fragile. It was so difficult to be in the CTICU that most parents only visited their sick babies for about an hour a day. The doctors encouraged Trisha to leave and rest since she just delivered a baby but she couldn't. She cried every time she left to pump milk, eat, or sleep a few hours. She was his mom and wanted to be with him. We had so many ups and downs and our emotions were raw.
Trisha and I have been seeking the help of a grief counselor. Because of what we went through, he told us that our bond with Nathan was much more than that of a typical parent & newborn baby. It's really hard to put this experience into words. We toured the CTICU and met with the doctors before we delivered but the experience was 10 times worse than we could have ever imagined. We hated being there but couldn't leave. 3 times a week, Erik would leave the hospital at 5am to drive home and get the kids. He would make the commute back to LA so that we could spend a few hours with them and then drive them back home, tuck them into bed, and drive back to the hospital once again. Trisha was exhausted from living in the ICU but Erik was equally tired from trying to stretch himself between the hospital and the kids at home. We were so happy when he was well enough to be transferred to CHOC and we thought that this nightmare would be over soon.
What happened on March 30th?
The day started off great. The ICU doctors did rounds that morning and all said that Nate looked great. All of his tubes were out with the exception of a one for his antibiotics. The cardiologist told us that his heart was functioning well and they were making plans to send him home within a day or two. The only thing that they were concerned about were his feedings. They told us that he needed to maintain full feedings in order to be released. Erik brought the kids up at about 10:30 that morning. Trisha met them in the hall and asked Erik to take the kids to the playroom for a while so that Nate could focus on his 11am feeding. When we were in Los Angeles, the kids weren't allowed to stay in his room for more than a few minutes, but at CHOC, we were able to spend time together as a family and the kids got lots of time to love on their brother. Because of that, his room was noisy at times and he sometimes got distracted eating. So, Erik and the kids went off to the playroom.
At 11am Trisha started giving Nate his bottle. He ate 1/2 of it really well and she sat him up to burp. As she did, Nathan began to struggle and his monitors started beeping. The nurse came in to see if everything was okay and within seconds, Nate turned blue from head to toe. She grabbed him out of Trisha's arms and pushed the CODE BLUE button. Within a minute, a dozen nurses, doctors and respiratory specialists were at his bedside. It was extremely chaotic. Trisha called Erik and told him that Nate was CODE BLUE and he needed to get up here. He left the kids with hospital volunteers and hurried upstairs. Together, we sat down in the back corner of the room and started praying. We asked God to let him live and begged him not to take him. The room became louder and more chaotic as the time went on. The doctors performed CPR and intubated him (breathing tube) and he came back --but his heart rate was sporadic and he was obviously in peril. As they did an echocardiogram, Nate was looking around the room and we were talking to him. We told him how much we loved him and we told him that he was going to be okay. The results of the echocardiogram were not good. They detected something--which they suspected was a large blood clot and before we were given an explanation doctors started yelling for a cut down tray. It was exactly like the traumas that we've seen on ER, only this was our kid and it was real. We were briefly told that they did not have time to get to the operating room and they handed us masks with instructions to put them on. Then, right in front of us they began operating on our baby boy. The hospital chaplain came in and sat with us. She repeatedly insisted that we call someone to start a prayer chain. Most everyone we knew was in church at the time so we just left a handful of messages. We kept thinking that any moment they were going to say that everything was fine. He was perfectly healthy just a few moments ago.
During the next hour, they frantically tried to save him. We kept hearing them call out for "more epy" and "more blood." His body temperature was too low so they were microwaving saline and trying to warm him up. We kept praying and pleading with God. There were glimpses of hope when the surgeon would say that they had a heartbeat but that was diminished when someone else would say he's losing too much blood. At 1:10 that afternoon, the doctors all became very quiet. One of them stepped over to us and told us that they were going to stop working on him because he was gone. We pleaded for them to keep trying but they said that all of the CPR had popped his heart and there was no hope. Then a doctor told us that "they stopped." Those were the two worst words that we've ever heard and at that moment we knew that life would never be the same again. Our Nathan Ryan was gone. His heart was broken and now ours was. It took them a few minutes to put him back together and then we were able to hold him. We were holding him but he wasn't there. We had to beg the doctors to take his breathing tube out and they told us that they needed permission from the Coroner. So Erik actually had to talk on the phone to the Coroner and after an hour or so, they took it out. We held him and kissed him and cried.
But the worst wasn't over. We still had to tell the kids what happened. We went to an empty room down the hall and one by one, they brought the kids in. We are supposed to protect them and now we had to tell them that their baby brother had died. They all cried and cried. It was devastating to see our kids in that much pain and there was nothing that we could do. Friends took the kids back to the playroom so that we could say goodbye to Nathan. We held him again and we asked our Pastor to dedicate him to God. The whole day was so surreal. A few hours ago they said that we could go home and now our son was dead. And the worst part about it was that we watched him die and there was nothing that we could do.
How are we doing (Trisha)?
So many people want to know how we are doing and we don't know how to answer that. We are just trying to get through each day and minimize the effect this has on us and the kids. We started going to a grief counselor the first week and have joined a support group through Saddleback Church. We are making every attempt to get through this knowing that we will never get over this. We hate being miserable and though it doesn't seem possible at this point, look forward to a day when we can be happy again. We've been told that the first year will be the hardest, specifically the first six months.
What we need
We are frequently asked what people can do to help. There's not a whole lot but here's a few things.
How are we doing (Erik)?
I'm doing one day at a time. Some days are better than others. It's been 73 days, and I still cry every day. Many things seem to remind me of Nathan; every helicopter, baby boys, Noah, medical stuff on TV, hospital/doctor bills, and on and on. It's difficult, because I make it a point not to break down in front of the kids. It still doesn't seem real. How could something so sad and unfair actually have happened? The counseling is helpful--we are really trying to lean into the grief process in the healthiest way possible both for us and the kids. I have been back to work for some time, but am admittedly less capable than before I left. We are doing more "normal" stuff--mostly events & activities for the kids.
I am hopeful that in time, we will find a new "normal," and that it will be a happy "normal." We really do have a lot to be thankful for & I try to focus on treasuring every day that God gives me with my family.
We really appreciate your support and your prayers.
While we were at CHLA, we tried to keep our email updates positive--but those 3 weeks were excruciating. After an 18 hour, 98% natural labor, Trisha ran a marathon trying to save Nathan's life. She spent 16-19 hours everyday sitting on an uncomfortable office chair next to Nathan, caressing his head (because he had tubes everywhere else) and telling him how much she loved him. Those hours were extremely stressful--starring at his monitors and as alarms went off throughout the day & night, and holding her breath as the doctors and nurses adjusted medications and machine settings to keep him alive. The staff worked around the clock caring for him. The (Cardio Thoracic Intensive Care Unit) CTICU was insane. There were critically ill babies all around recovering from open heart surgery. Alarms and bells went off around the clock--Nathan was extremely fragile. It was so difficult to be in the CTICU that most parents only visited their sick babies for about an hour a day. The doctors encouraged Trisha to leave and rest since she just delivered a baby but she couldn't. She cried every time she left to pump milk, eat, or sleep a few hours. She was his mom and wanted to be with him. We had so many ups and downs and our emotions were raw.
Trisha and I have been seeking the help of a grief counselor. Because of what we went through, he told us that our bond with Nathan was much more than that of a typical parent & newborn baby. It's really hard to put this experience into words. We toured the CTICU and met with the doctors before we delivered but the experience was 10 times worse than we could have ever imagined. We hated being there but couldn't leave. 3 times a week, Erik would leave the hospital at 5am to drive home and get the kids. He would make the commute back to LA so that we could spend a few hours with them and then drive them back home, tuck them into bed, and drive back to the hospital once again. Trisha was exhausted from living in the ICU but Erik was equally tired from trying to stretch himself between the hospital and the kids at home. We were so happy when he was well enough to be transferred to CHOC and we thought that this nightmare would be over soon.
What happened on March 30th?
The day started off great. The ICU doctors did rounds that morning and all said that Nate looked great. All of his tubes were out with the exception of a one for his antibiotics. The cardiologist told us that his heart was functioning well and they were making plans to send him home within a day or two. The only thing that they were concerned about were his feedings. They told us that he needed to maintain full feedings in order to be released. Erik brought the kids up at about 10:30 that morning. Trisha met them in the hall and asked Erik to take the kids to the playroom for a while so that Nate could focus on his 11am feeding. When we were in Los Angeles, the kids weren't allowed to stay in his room for more than a few minutes, but at CHOC, we were able to spend time together as a family and the kids got lots of time to love on their brother. Because of that, his room was noisy at times and he sometimes got distracted eating. So, Erik and the kids went off to the playroom.
At 11am Trisha started giving Nate his bottle. He ate 1/2 of it really well and she sat him up to burp. As she did, Nathan began to struggle and his monitors started beeping. The nurse came in to see if everything was okay and within seconds, Nate turned blue from head to toe. She grabbed him out of Trisha's arms and pushed the CODE BLUE button. Within a minute, a dozen nurses, doctors and respiratory specialists were at his bedside. It was extremely chaotic. Trisha called Erik and told him that Nate was CODE BLUE and he needed to get up here. He left the kids with hospital volunteers and hurried upstairs. Together, we sat down in the back corner of the room and started praying. We asked God to let him live and begged him not to take him. The room became louder and more chaotic as the time went on. The doctors performed CPR and intubated him (breathing tube) and he came back --but his heart rate was sporadic and he was obviously in peril. As they did an echocardiogram, Nate was looking around the room and we were talking to him. We told him how much we loved him and we told him that he was going to be okay. The results of the echocardiogram were not good. They detected something--which they suspected was a large blood clot and before we were given an explanation doctors started yelling for a cut down tray. It was exactly like the traumas that we've seen on ER, only this was our kid and it was real. We were briefly told that they did not have time to get to the operating room and they handed us masks with instructions to put them on. Then, right in front of us they began operating on our baby boy. The hospital chaplain came in and sat with us. She repeatedly insisted that we call someone to start a prayer chain. Most everyone we knew was in church at the time so we just left a handful of messages. We kept thinking that any moment they were going to say that everything was fine. He was perfectly healthy just a few moments ago.
During the next hour, they frantically tried to save him. We kept hearing them call out for "more epy" and "more blood." His body temperature was too low so they were microwaving saline and trying to warm him up. We kept praying and pleading with God. There were glimpses of hope when the surgeon would say that they had a heartbeat but that was diminished when someone else would say he's losing too much blood. At 1:10 that afternoon, the doctors all became very quiet. One of them stepped over to us and told us that they were going to stop working on him because he was gone. We pleaded for them to keep trying but they said that all of the CPR had popped his heart and there was no hope. Then a doctor told us that "they stopped." Those were the two worst words that we've ever heard and at that moment we knew that life would never be the same again. Our Nathan Ryan was gone. His heart was broken and now ours was. It took them a few minutes to put him back together and then we were able to hold him. We were holding him but he wasn't there. We had to beg the doctors to take his breathing tube out and they told us that they needed permission from the Coroner. So Erik actually had to talk on the phone to the Coroner and after an hour or so, they took it out. We held him and kissed him and cried.
But the worst wasn't over. We still had to tell the kids what happened. We went to an empty room down the hall and one by one, they brought the kids in. We are supposed to protect them and now we had to tell them that their baby brother had died. They all cried and cried. It was devastating to see our kids in that much pain and there was nothing that we could do. Friends took the kids back to the playroom so that we could say goodbye to Nathan. We held him again and we asked our Pastor to dedicate him to God. The whole day was so surreal. A few hours ago they said that we could go home and now our son was dead. And the worst part about it was that we watched him die and there was nothing that we could do.
How are we doing (Trisha)?
So many people want to know how we are doing and we don't know how to answer that. We are just trying to get through each day and minimize the effect this has on us and the kids. We started going to a grief counselor the first week and have joined a support group through Saddleback Church. We are making every attempt to get through this knowing that we will never get over this. We hate being miserable and though it doesn't seem possible at this point, look forward to a day when we can be happy again. We've been told that the first year will be the hardest, specifically the first six months.
One very hard part of this is the isolation. Because no one knows what to say to us, most people just stay away or pretend they don't see us when we're out. People think that they're doing us a favor by "giving us space" but it's really hard to be so alone. We know that it's hard for people to be our friends right now. We're not very fun to be around. We are doing normal things, like taking the kids to school and sports, but life is far from normal. I have moments of happiness and laughter but that is short lived with the memory of what happened constantly racing around in my mind. In fact, the empty hole in my heart makes it impossible for me to think of anything else for more than a few minutes.
Every time I leave my house, I get all worked up in anticipation of what people are going to say. Most people just ignore me but many others say "how's it going" with enthusiasm like nothing ever happened, and others seem to need confirmation that we're doing okay -- something that I can't give them. We've experienced a very traumatic event that was prefaced by 25 days of extreme insanity. We don't expect people to get the full nature of what we've been through which is why we are posting this blog. We need people to understand where we've been, and why we are not capable of being normal right now. In fact, we need to find a new normal because life is never going to be the same again. We need people to "get it" so that we can feel safe leaving our house and supported in our grief. We still don't know why Nathan died. We've had to speak with the Coroner a few times and have forwarded a copy of the autopsy report up to our doctors at CHLA. We hope to understand what happened but there is a possibility that we will never know.
Another thing that I struggle with is that there seems to be babies everywhere. I realize that there are an abundance of babies in Ladera Ranch, but it really seems like they follow me around. It's so painful to see someone holding their baby--I can't even begin to explain it. That's what I'm supposed to be doing right now and instead, my baby is six feet underground. That pain is so intense right now that I try as hard as I can to avoid being around babies. I hope that those of you that have little ones can understand and give me a little grace with this.
What we need
We are frequently asked what people can do to help. There's not a whole lot but here's a few things.
- Keep in contact. We do appreciate emails and phone messages. We may not return calls or emails but it is really comforting to know that people are still thinking about us. And, some days we appreciate an invitation to get together, we just don't know when or how often those days will come.
- Meals. I feel like it's ridiculous to ask for help with this but I still need it. I never realized how physical grief is. It sucks up a significant portion of our energy. Our counselor told us as much as 75% -which is why we feel so wiped out all the time. It's hard to take care of 4 kids right now and I just don't have much energy or desire to go to the grocery store or make dinner every day. So, we really appreciate it when someone takes the time to bring us a meal. Diane Hall at church is coordinating meals. If you want to contact her, her email is hall_diane@email.com.
- What to say. I know that people walk on eggshells around us not knowing what to say. I'm just as uncomfortable and I don't know what to say as well. But, it is hard to always feel so alone. I must admit that I hate it when people say "how's it going?" when we are out. I realize that's the standard conversation for our society but it puts me immediately into a high stress situation where I don't know what to say. I doubt that most people really want to know how crappy my day was and I'm not capable of saying the societal acceptable answer of "good". Instead, just say, "hi" or, "it's good to see you."
How are we doing (Erik)?
I'm doing one day at a time. Some days are better than others. It's been 73 days, and I still cry every day. Many things seem to remind me of Nathan; every helicopter, baby boys, Noah, medical stuff on TV, hospital/doctor bills, and on and on. It's difficult, because I make it a point not to break down in front of the kids. It still doesn't seem real. How could something so sad and unfair actually have happened? The counseling is helpful--we are really trying to lean into the grief process in the healthiest way possible both for us and the kids. I have been back to work for some time, but am admittedly less capable than before I left. We are doing more "normal" stuff--mostly events & activities for the kids.
I am hopeful that in time, we will find a new "normal," and that it will be a happy "normal." We really do have a lot to be thankful for & I try to focus on treasuring every day that God gives me with my family.
We really appreciate your support and your prayers.
Subscribe to:
Posts (Atom)